Tackling the Inverse Care Law: Reducing health inequalities in Wales through General Practice and place-based partnerships
February 5, 2025
Following the webinar Inverse Care Law in Wales: A Way Forward, this spotlight feature looks at examples of the Inverse Care Law in Wales, alongside strategies and initiatives across Wales which aim to reduce inequalities through General Practice and place-based partnerships.
This spotlight feature includes case study contributions from Deep End Cymru, The North Wales Inverse Care Law Programme and the Primary Care Division of Public Health Wales.
What is the Inverse Care Law?
The principle of the Inverse Care Law is that the availability of good medical care often varies inversely with the need for it in the population served.
In primary care, deprived patients have been shown to have reduced access to scheduled consultations and to spend less time with GPs during consultations than more affluent patients (Pedersen and Vedsted, 2014). Patients in deprived areas who lack the health literacy, confidence, and agency are less likely to seek referral, whereas affluent patients are more likely to demand it (Watt, 2018).
The inverse care law is more apparent where medical care is most exposed to market forces, and less so where exposure is reduced (50 years of the inverse care law, The Lancet).
The law was introduced in a paper authored by Julian Tudor Hart, titled The Inverse Care Law, published in 1971. Tudor Hart observed that disadvantaged populations need more health care than advantaged populations, but received less.
The Inverse Care Law is primarily about inequity in healthcare that results in unfair social inequalities in health.
Case study 1 Deep End Cymru: General Practice at its best where it’s needed most
One of the Five Essential Conditions to reduce health inequities is Health Services, and most of the effective interventions that make a difference at population level are delivered through primary care.

Figure 1 The fives essential conditions needed to live a healthy, prosperous life (WHO Europe, 2019).
The best primary care should be provided for those who would most benefit. However, the Inverse Care Law in primary care is still very apparent in Wales, with evidence of deprived communities receiving less care than more affluent communities.
The project invited the 100 (of all 389 GP practices in Wales) that had the highest proportion of their patients living in the most deprived 20% of communities to join Deep End Cymru. These practices reach almost 60% of the 653,413 people living in the most deprived parts of Wales. The project found evidence of an Inverse Care Law in resources such as funding and workforce – they have a greater workload and a smaller workforce.
For example, GP partners in the Deep End have on average, 764 (29.7%) more patients than those in the 100 least Deep End practices. This results in significant unfairness for patients in terms of the time and energy available of the people caring for them in their GP surgery. What can we do about this embedded inequity in health care provision?
Figure 2 Deep End GP Practices in Wales
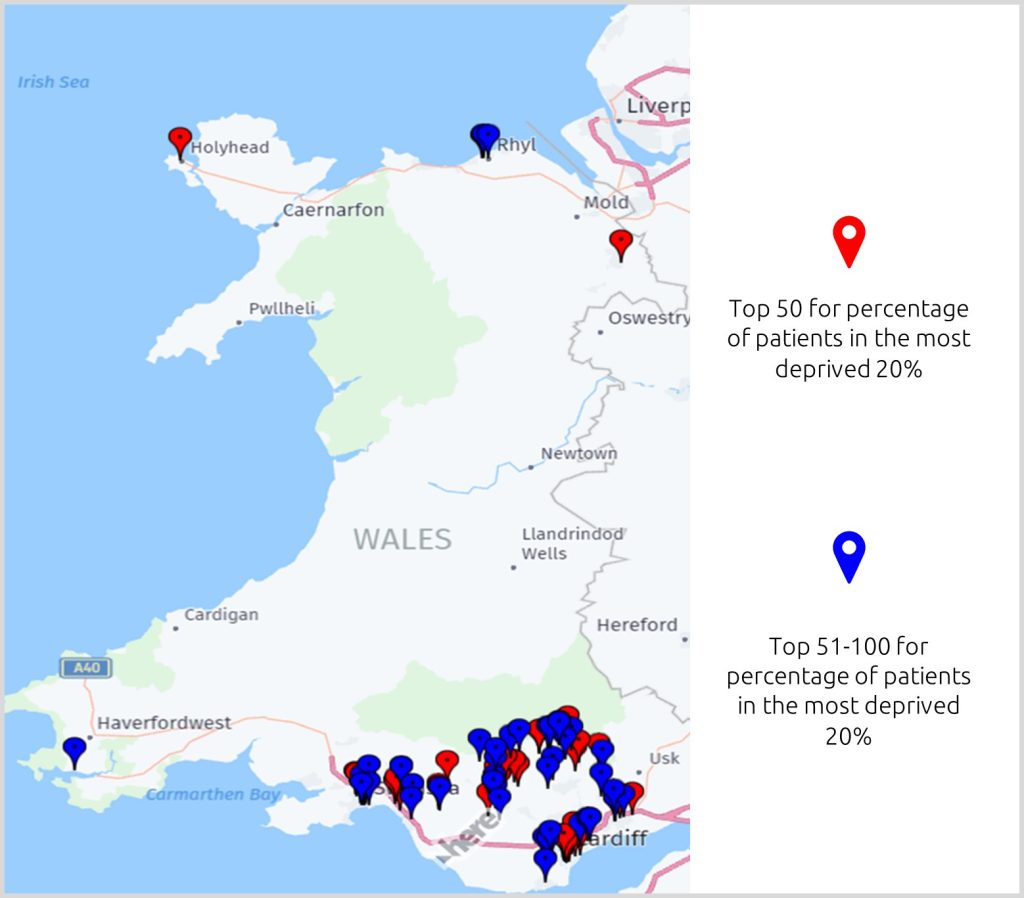
Source: Stats Wales | General practice population
What does Deep End Cymru do?
The Deep End movement began in Scotland in 2009 and has extended to multiple programmes in the UK and internationally, including most recently, in Wales where Deep End Cymru launched in late 2022, hosted by the Royal College of General Practitioners (RCGP) and funded by Welsh Government.
Deep End Cymru is a grassroots movement developing mutual support to generate change to improve healthcare services and health outcomes for people with the greatest health needs. It is a way to bring a stronger health equity lens to all business as usual, for example, in Cluster plans and Social Prescribing programmes. It aims to add value for those communities who are often less able to access and benefit from existing services. Deep End Cymru invited front line primary care staff to meet in protected time to explore their common challenges and possible solutions. The following themes were covered: Workforce, Education, Advocacy and Research (WEAR).
Deep End Cymru have:
- Explored solutions to non-medical needs and are developing a business case for Deep End link workers.
- Worked with Health Education and Improvement Wales (HEIW) on how training and education for all primary care team members can pivot to include deprivation medicine.
- Created strong links with Cardiff University with research activities, including a qualitative study into working in the Deep End, and a study on Exploring the equity of distribution of general medical services funding allocations in Wales: a time-series analysis | BJGP Open.
- Used knowledge to advocate for our communities and staff.
Concluding remarks from Deep End Cymru
General Practice is in crisis in Wales and this is having an even greater impact on communities where the GP surgery is a lifeline when so many other services have shrunk away. Deep End participants say they love working in their practices and are highly motivated to making a difference to families and communities who most need them.
The Deep End network is trying to give a voice to those who often have great ideas for solutions that the whole health system would benefit from. Deep End Cymru have generated a resource of great ideas and are putting them into practice at pace.

Deep End practices are more likely to close, merge or be taken over by external companies. Deep End Cymru has a role in advocacy for practices that have the least time to do this for themselves and are at greatest risk of folding, leaving their patients at an even greater disadvantage.
If you are interested to help, please see Deep End Wales Project, and Deep End Cymru Report First Phase 2024 And contact DeepEndWales@rcgp.org.uk
Case study 2 The Inverse Care Law Programme – reducing health inequalities in North Wales
In North Wales, males living in the most deprived areas can expect to live around 12 years less in good health compared with those in the least deprived areas with nearly an 11 year difference in females. The gap in life expectancy at birth between the most and least deprived areas is 7 years for males and 6 years for females (Public Health Outcomes Framework, Public Health Wales, 2025).
Figure 3 Welsh Index of Multiple Deprivation (WIMD) 2019, Wales
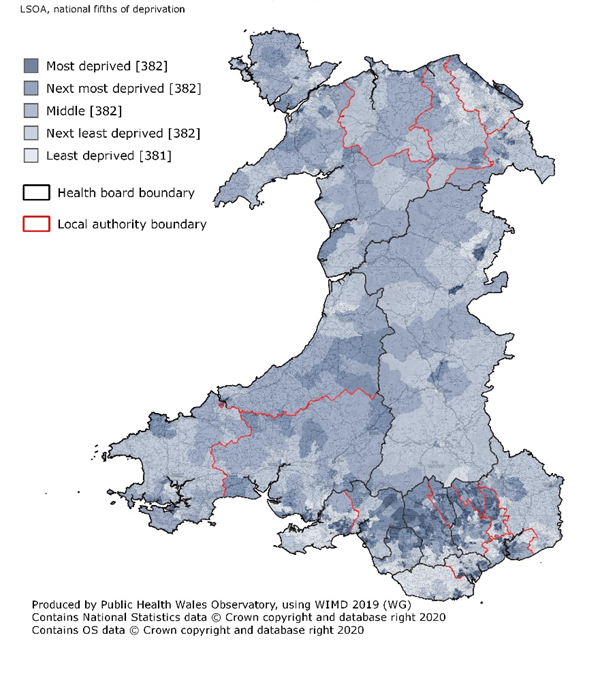
Table 1 The 10 most deprived Lower Super Output Areas (LSOAs) in North Wales
| Local authority | LSOA | WIMD Rank* |
| Denbighshire | Rhyl West 2 | 1 |
| Denbighshire | Rhyl West 1 | 2 |
| Wrexham | Queensway 1 | 9 |
| Denbighshire | Rhyl West 3 | 11 |
| Denbighshire | Rhyl South West 2 | 19 |
| Conwy | Glyn (Conwy) 2 | 20 |
| Wrexham | Wynnstay | 45 |
| Denbighshire | Rhyl South West 1 | 57 |
| Conwy | Abergele Pensarn 2 | 70 |
| Conwy | Tudno 2 | 78 |
Further information on WIMD available at: https://www.gov.wales/welsh-index-multiple-deprivation
The North Wales Inverse Care Law Programme
Betsi Cadwaladr University Health Board have led an innovative programme of work to kick start a systems approach to addressing local health inequalities and to create a healthier north Wales. The aim was to create a place-based, partnership approach to reducing health inequalities with an approach from the outset recognising that social, economic and environmental determinants have a significant impact on health but are beyond the scope of the NHS to address.
The Programme worked with three innovator primary care clusters who had expressed an interest to be involved.
Cluster map available here.
Three one day workshops were held in each of the three clusters in September, October and November 2023 involving over 60 local partners across the three clusters. The workshops focused on building knowledge about health inequalities and the system, looking at local data and intelligence through a bespoke dashboard then encouraged the development of at least 38 projects or innovations (across three clusters) focusing on tackling health inequalities.
Lived experiences and stories from those involved, enabled true collaboration and an appetite to change the status quo. Innovation examples included food poverty collaborations, the development of guidance to promote inclusive care for homeless people and preventative initiatives through collaboration between the Stroke Prevention Team and other organisations such as Mind and farmer’s markets.
Evaluation and Impact: Opportunities and challenges of the programme
The Programme was evaluated externally by Urban Foresight. A link to the full report is available here. The evaluation demonstrated that the programme achieved its overall aim and is a blueprint for what is needed to develop and enable a place-based, partnership approach to reducing health inequalities.
Financial challenges meant there was no additional financing available to clusters to support their innovations. With this in mind, the resilience of people, communities, stakeholders and organisations was commendable and their ability to use assets and resources already placed in communities became the focus of work demonstrating the important outcome of protecting and using already available assets.
Limitations to continuing to develop the innovations include financial limitations, workforce and time – much of the work is being embedded into an already stretched workforce across all organisations.
Details of the evaluation conducted by Urban Foresight, available at: Tackling health inequalities in Wales – Urban Foresight

Concluding remarks from the North Wales Inverse Care Law Programme
This programme of work has successfully built on shared capabilities, assets, insights, and relationships across sectors and has encouraged and inspired local innovation across the three innovator clusters. It has built capabilities across the system, led to new connections, encouraged innovation, and supported more efficient ways of working. Those working in local communities have joined forces with a true appetite and purpose to reduce health inequalities through partnership working while considering the wider determinants contributing to these inequalities. It is hoped that this innovative approach will bring us a step closer to long lasting change in our approaches to ways of working and enable consideration to a change in mindsets to bring sustainability to primary and community care.
Case study 3 Reducing Health Inequalities in Primary Care (Primary Care Division, Public Health Wales)
In early 2023 the Primary Care division brought together key data form across Wales to demonstrate how despite the well documented increased needs in some of our communities the provision of doctors, nurses and other staff is lower. The Inverse Care Law still exists in Wales. There has been growing evidence for the last 50 years on how primary care can help to tackle these inverse care laws. Dr Julian Tudor-Hart was one of the first to describe some of these methods. Although he acknowledged that a GP has limited ability to tackle deprivation there is much that can be done form the role and by understanding the community and patients’ lives, it can help the GP to deliver high quality effective primary care which can produce better health outcomes and help to mitigate some of these broader determinants. Using his deep knowledge of the community and his patients, he focused on prevention, early intervention and best evidence treatments, and implemented these through local cooperation.
With the legacy of Dr. Hart in mind, the Health Inequalities Programme of Primary Care is working to embed health inequalities within the Primary Care system in Wales. Since its establishment in the last quarter of 2023, the programme has reached out to a wide range of partners and stakeholders across Wales and developed a variety of resources to enable primary care to tackle health inequalities and the Inverse Care Law including, data and intelligence, a series of case studies and evidence reviews, training resources for health professionals including educational directory for health professionals, a series of webinars for primary care on health inclusion, and a health equity self-assessment toolkit for primary care. A link to the newly developed webpages is available here.
We are currently in the process of developing an Action Framework for primary care to address health inequalities. Three in person stakeholder workshops were held in October 2024 to co-develop key action areas. The conversation is ongoing with additional online workshops with key stakeholders and service users, in early 2025 with the expectation that an action framework with a strategic action plan will be developed by April 2025.
A hackathon challenges proposed by the Primary Care Division of Public Health Wales is also underway by the NHS Wales Modelling Collaborative. The challenge being supported by a steering group is looking into Feasibility for identification of chronic conditions at cluster and health board levels that have highest impact on increasing health inequalities in Wales. For further information about the inequalities programme or if you would like to be involved in any aspect of the programme, please contact us via email pcd.business.support@wales.nhs.uk
The webinar is available to view here.
Useful resources
- Deep End Cymru webpage. Available at: Deep End Wales Project
- Safe surgeries: Safe Surgery can be any GP practice which commits to taking steps to tackle the barriers faced by many migrants in accessing healthcare. Available at: Safe Surgeries – Doctors of the World
- Reducing Health Inequalities through Primary Care. Available at: Reducing Health Inequalities through Primary Care – Primary Care One
- Wales Inclusion Health Programme for Primary Care. Available at: Wales Inclusion Health Programme for Primary Care – Primary Care One
- Health Equity Evidence Centre. Available at: Welcome to the Health Equity Evidence Centre – Health Equity Evidence Centre
- Evaluation of the Betsi Cadwaladr UHB Inverse Care Law Programme. Available at: Tackling health inequalities in Wales – Urban Foresight