Using Behavioural Science to Tackle Health Inequalities
November 3, 2025
Introduction to Behavioural Science and the BeSci Unit
Behavioural science is the study of human behaviour, noting the mix of cognitive, psychological, social, and environmental factors that affect it, and how these can vary by population group. It helps us understand what supports and/or stops people taking action that might affect their health, and how we can best support them to make healthier choices. In public health, behavioural science is especially valuable in shaping policies, services, and communications to be more effective, inclusive, and equitable.
The Behavioural Science (BeSci) Unit at Public Health Wales provides specialist expertise to integrate behavioural science into public health practice. The Unit supports public health professionals, policymakers, and service designers to:
- Apply behavioural insights to improve health and wellbeing outcomes,
- Develop behaviourally informed resources and projects,
- Build their capacity and capability, across the public health system,
- Collaborate across sectors and academic institutions to design better interventions.
The BeSci Unit plays a key role in helping to design interventions that reduce health inequalities by considering real-world behavioural challenges and barriers faced by different population groups and using approaches that help overcome them.
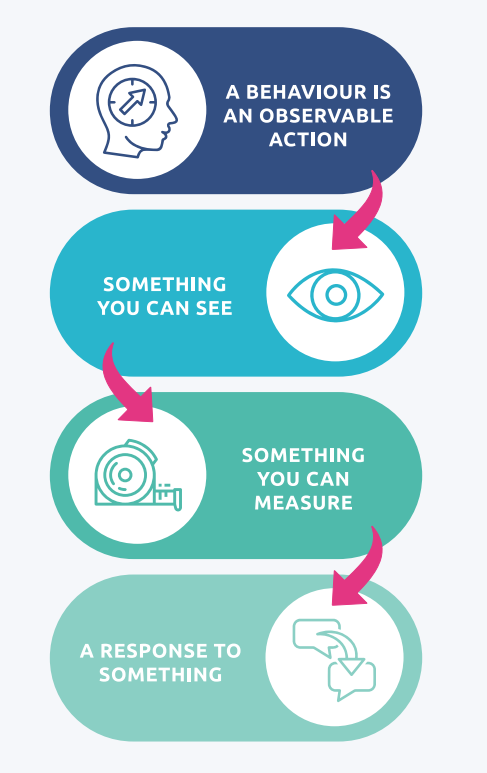
Figure 1: What is a behaviour
Understanding the Problem
A major public health challenge is that universal health interventions often don’t work equally well for everyone. A programme aimed at improving screening or vaccine uptake might succeed in one community but have little effect in another. These differences often reflect unequal levels of personal agency, a person’s ability to make changes in their life or environment to benefit from a health intervention.
Because many public health interventions are developed quickly and under pressure, especially in primary prevention, they often take a universal approach, applying the same strategy across the whole population. These interventions typically have a high agentic demand: they rely heavily on individuals taking initiative and action.
But personal agency is not evenly distributed. It depends on:
- Individual capacity – knowledge, skills, and confidence
- Resources – financial, material, and social support
- Freedom and opportunity – the ability to act on health-promoting choices
If these factors are not considered and addressed in design, interventions with high agentic demand can unintentionally widen health inequalities.
| Level of demand | Description | Example | Outcome variants |
| High | Interventions that require individuals to take personal responsibility for change. These rely on people having the knowledge, motivation, time, and resources (such as money or cognitive effort) to act. | A public health campaign encouraging people to eat less salt through better food choices. | Success depends on individual awareness, understanding, and ability to change behaviour. |
| Low | Interventions that reduce the burden on individuals by changing the environment, systems, or social norms in which behaviours occur. These approaches make healthy choices easier or automatic, requiring minimal personal effort. | Reformulating processed foods to reduce salt content. | Everyone benefits without needing to make an active choice or take action. |
Table 1: Agentic demand (Garrott 2023)
A clear example of this issue can be seen in obesity prevention policy in England. Over the past 30 years, only 19% of nearly 700 proposed policies had low agentic demand. The rest relied heavily on personal action, rather than system-level support.
Solutions-Based Action: How Behavioural Science Can Help
Behavioural science helps reframe and redesign interventions so that they can:
- Consider the behavioural realities of the people they aim to serve,
- Reduce the demands placed on individuals,
- And ultimately become more equitable and effective.
By applying behavioural science early in the design process, we can build public health solutions that deliver what we aim for, more often.
The BeSci Unit supports this process by:
- Embedding behavioural science into public health policy, services, and communication,
- Offering approaches, for example to help create behavioural specifications to clarify the “who, what, when, and where” of an intervention,
- Helping identify when and how behavioural challenges may reinforce or tackle inequalities, and
- Working across sectors to ensure joined-up, evidence-based approaches.
An example of how BeSci was applied in practice comes from the Help Me Quit Smoking Cessation Service. Communication to some clients who self-refer to Help Me Quit is done via SMS message. The SMS aims to prompt clients to engage with support services after they initiated a self-referral via the website. Engagement data showed that only 5% of clients who received the original SMS called the service on Day 0. Overall, the rate for successful contact from those that self-referred was 30%. Many clients did not respond to the service’s attempts to engage, likely due to the lack of an immediate call-to-action, or motivational framing. BeSci applied behavioural specification (Figure 2) to identify the who, what, when and where of the intervention.
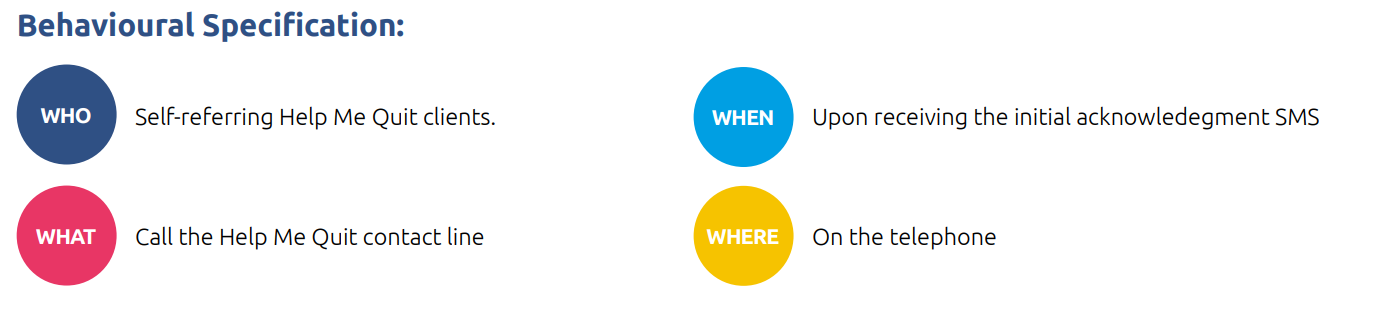
Figure 2. Behavioural Specification for the Help Me Quit Campaign (BeSci Case Studies)
Positive framing and providing a timely prompt to ensure client motivation was not lost. Overall, this helped to shift the messaging from purely informative communication to action-oriented messaging that is more likely to derive target behaviour change. Helping more smokers to quit has clear benefits to individuals, but it’s also important in terms of health equity – the death rate linked to smoking in those from the most disadvantaged areas is more than three times higher than in those from the least disadvantaged areas.
| Original communication: | Amended communication: |
| Hi [%FORENAME%], you requested a call back from Help Me Quit. A member of our team will call you soon to talk about how we can support you. Alternatively call us on 0800 0852219 at a time suitable for you. We’re open Mon/Wed 9am-8pm, Tue/Thur 9am-6pm, Fri/Sat 9am-5pm. Reply STOP to cancel | Hi [%FORENAME%], well done on starting your quit journey! Call us today on 0800 085 2219 to take the next step and plan your path to being smoke-free. We’re open Mon/Wed 9am-8pm, Tue/Thur 9am-6pm, Fri/Sat 9am-5pm. Why not make today the day? If you’re unable to call, we’ll be in touch soon. Reply STOP to cancel. |
Table 2: Help Me Quit – SMS Text Messages (Behavioural Science Unit)
Conclusion
Addressing health inequalities requires a deeper understanding of how behaviour is shaped by real-life contexts and designing public health solutions that reflect that reality – in clearly defined target population groups. Effective interventions should account for the requirement of conscious effort (how hard it is for people to take the required actions, like changing habits or making decisions), because not everyone has the same ability or resources to do so. For example, using personalised risk profiles can help influence behaviours like smoking and diet but places greater responsibility on the individual. In contrast, changing the context or choice architecture, such as increasing the availability of healthier food options, requires less effort from individuals and can lead to more equitable outcomes.
Making services more responsive to the needs and preferences of diverse populations, by changing default options or simplifying complex systems has been shown to improve the uptake of preventive health services. Choosing the right mechanism for a given intervention requires active consideration of agentic demand, ideally through starting with a clear behavioural specification, then diagnostic and design processes. This approach helps ensure that interventions reduce health inequity, or at the very least, do not worsen it.
To support this work, Public Health Wales offers:
- An over-arching guide
- A suite of associated tools
- An online repository of case studies and resources
- A Community of Practice (CoP) for Wales, open to anyone interested in improving the impact of policies, services, and communications through the routine application of behavioural science
The work of the BeSci Unit demonstrates that when behavioural science is systematically applied, it enables smarter, fairer, and more effective health interventions.
References
- Development and application of the Demands for Population Health Interventions (Depth) framework for categorising the agentic demands of population health interventions. BMC Global and Public Health. Available at: https://bmcglobalpublichealth.biomedcentral.com/articles/10.1186/s44263-024-00043-8
- What types of interventions generate inequalities? Evidence from systematic reviews. Journal of Epidemiology & Community Health. Available at: https://jech.bmj.com/content/67/2/190
- Blueprint For the Use of Social and Behavioral Science to Advance Evidence-Based Policymaking, Subcommittee on Social and Behavioral Sciences of the Committee on Science of the National Science and Technology Council, May 2024. White House OSTP Releases Blueprint for the Use of Social and Behavioral Sciences for Evidence-based Policymaking
- The impact of communicating genetic risks of disease on risk-reducing health behaviour: systematic review with meta-analysis. BMJ. Available at: https://www.bmj.com/content/352/bmj.i1102
- Impact of increasing the proportion of healthier foods available on energy purchased in worksite cafeterias: a stepped wedge randomized controlled pilot trial. Appetite. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC6335439/pdf/main.pdf
- Behaviourally Informed Communications Initiative (BICI): Case Studies. Available at: Behaviourally-Informed-Communicaitons-Initiative-BICI-Case-Studies.pdf